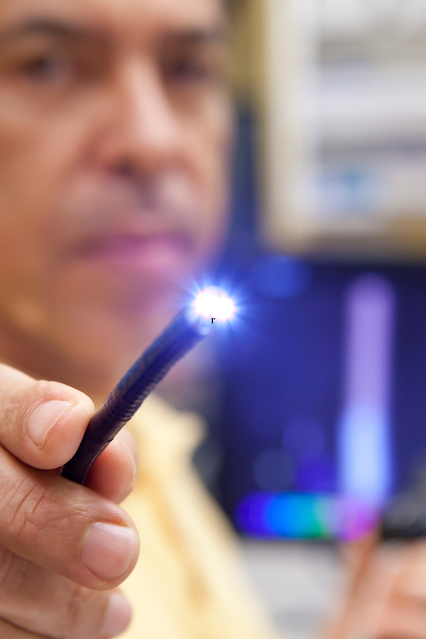
An endoscopy is a minimally invasive medical procedure that involves inserting an endoscope—a long, thin tube with a camera—into your body to examine your tissues or internal organs. Normally, the endoscope is inserted through natural openings like your mouth, but your doctor can make small incisions in other parts of your body such as your abdomen or knees for the tube to pass through.
Doctors often recommend an endoscopy to investigate symptoms or
confirm a diagnosis, but such procedures can also be used as a form of
treatment. For instance, an endoscopy may be administered to remove polyps or
cauterise bleeding vessels. Some endoscopies can even be administered together
with other procedures such as ultrasound scans.
There are various types of endoscopy procedures, including upper
endoscopy (for the inner lining of your digestive tract) and colonoscopy (for
checking your bowels). The latter
happens to be quite common, and it’s often used to diagnose and preemptively
treat colorectal cancer by removing potentially harmful polyps. With this,
colonoscopies can be life-saving procedures since they help prevent the
worsening of colorectal cancer—the United States’ second most common cancer
death and the leading type of cancer in Singapore.
That said, there are some myths about endoscopies that many
people still believe. In this article, we’ll debunk these myths to give you
some insight into what exactly these procedures are all about.
Myth 1: Endoscopies Require
Lengthy Stays at the Hospital
Most endoscopies are outpatient procedures, which means that
patients are allowed to go home within the day. After the procedure, your
doctor will stitch up your incision wounds and give you tips on how to treat
them. Then, you will likely stay at the hospital for up to two hours to rest
your body and wait for the sedative effects to die down.
Myth 2: Endoscopies Are Painful
For the most part, endoscopies are not painful. Often, doctors
will give patients an anaesthetic or a light sedative to prevent discomfort
during the procedure. For colonoscopies, you might feel some cramping or
pressure, mostly due to the air used to expand your colon to give way for
analyses. Most likely, you won’t remember going through the procedure at all.
However, some procedures might result in discomfort for a few
days. An upper gastrointestinal tract (GI) endoscopy, for instance, might leave
you with a sore throat and require you to eat soft foods over the next few
days. Some cystoscopies (endoscopy for the bladder via your urethra) may also
cause blood in your urine over the next 24 hours. These side effects typically
go away on their own, but you can always consult your doctor for treatment
tips, especially if the symptoms persist.
Myth 3: The Preparation Is Too
Hard
For endoscopies, especially colonoscopies, patients are advised
to drink a solution for bowel preparation. This solution is meant to induce
your bowel movements and clear out your colon. In recent years, bowel prep
solutions underwent changes to become better-tasting than the ones used in the
past. Prep solutions are typically flavourless, but some doctors recommend
mixing them with soda for a more palatable taste. Drinking bowel prep solutions
are important since they help ensure a clear overview of your colon so that
doctors won't miss any potential cancerous growths.
Myth 4: Endoscopies Are Risky
Endoscopies are generally safe, but there are extremely rare
cases of perforation that may require surgery. For instance, it’s possible that
the endoscope used for a colonoscopy might puncture your rectum, intestine, or
colon. Still, it should be noted that these scenarios are highly unlikely. One
study suggests that the risks of perforation are 4 per 10,000 while the risks
of major haemorrhage are 8 per 10,000.
Rectal bleeding is another rare occurrence that might follow a
colonoscopy and the removal of a polyp. However, this symptom is often very
minor and goes away on its own after a few days.
Myth 5: Endoscopies Are
Embarrassing
A reputable hospital with a trusted medical staff would know how
to be respectful and professional when it comes to procedures of this nature.
Other than that, the doctors, nurses, and staff have likely done endoscopies
numerous times, enough to understand the need for patient discretion. These
professionals are comprehensively trained to prioritise your privacy, comfort,
and well-being, especially with sensitive medical procedures.
Myth 6: Only Men Need
Endoscopies
Endoscopies, particularly colonoscopies, are often linked to
older men. Although it’s true that colorectal cancer is more prevalent among
men, that doesn’t mean women should pass on colonoscopies already. Colorectal
cancer is still a common condition, and colonoscopies will help men and women
stay on top of their health and regularly check for signs of cancer.
In addition, there are other types of endoscopies that women may
benefit from. Hysteroscopy, which is meant to examine the womb, helps doctors
investigate symptoms such as pelvic pain, postmenopausal bleeding, heavy
periods, fertility-related complications, and fibroids or polyps in the womb.
The Bottom Line: Endoscopies are
Safe and Essential
All in all, endoscopies are safe procedures that are unlikely to
bring you severe pain and discomfort. They can be done quickly and are vital
for investigating, confirming, and treating issues with your internal organs.
Sometimes, your doctor might schedule subsequent check-ups after the procedure
to monitor signs of side effects such as fever, bleeding, or pain. Overall,
endoscopies shouldn’t be a cause for concern. Rather, they should be thought of
as wise preventative measures for potentially life-threatening complications.



Post a Comment